By Nihal Said, Research & Partnerships Senior Advisor & Harjyot Khosa, External Relations Director of IPPF South Asia
‘Can I just take the abortion pills along and have it in my home?’ Asked young Meera, as we sat in Bhaktapur young people drop-in center in Nepal. ‘We have everything on our phone and can access it, once we are in a safe space,’ added Meera.
In an ideal world, we would tell Meera, yes you can take abortion pills from a provider or from a pharmacy and use them when you need, where you feel safe, and seek help and support from a provider when needed. In an ideal world, services would be available to those who needed without permission to access and can be sufficient to fulfil health needs. But we are not yet in this ideal world, and despite calls to centre care on people, self-care is not mainstreamed effectively. According to a 2022 qualitative study in Nepal among sexual and reproductive health service users and providers, there were different barriers identified by users such as poor awareness of self-care methods for SRH and perceived lack of need for self-care, limited access to medicines or guidance as well as negative behaviors from the service providers (Timilsina, Amit et al. , 2024). These barriers experienced by clients and young people demonstrate the need for upholding the commitments to rights based sexual and reproductive healthcare where self-care is an integral part and not an optional or selective modality to access services.
when
Subject
Sexual Health

Can I just take the abortion pills along and have it in my home?
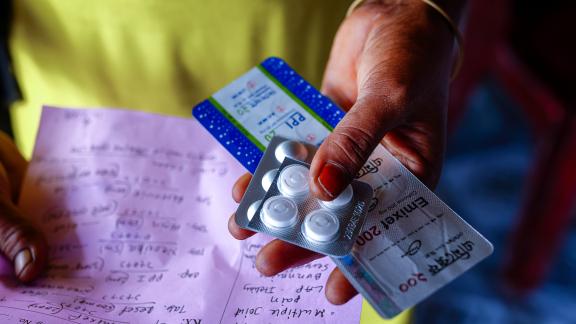
IPPF / Uma BistaSelf-care is about promoting individual and collective health and wellbeing. It includes self-awareness, self-testing and self-management of healthcare needs. (WHO, 2024). Self-care interventions within sexual and reproductive health could include self-injection (e.g., of contraceptives), self-screening or testing (e.g., for sexually transmitted infections and pregnancy), self-sampling (HPV for cervical screening), self-medication (e.g., for medical abortion and HIV), self-monitoring (e.g., of fertility) and the use of lubricants for sexual health and well-being. Within IPPF and in relation to abortion self-care, it is the right of women, girls and all people who can become pregnant to lead, in part or entirely, their abortion process, with or without support from health providers (IMAP statement, 2021). These perspectives on self-care call for removing all barriers to accessing rights-based and high-quality sexual and reproductive health services.
Person-centred care is inclusive of self-care and leverages all entry points to care including in-person care and digital health interventions when needed by clients. Self-care doesn’t relieve the health system of the legal and professional obligations that safeguard clients accessing services. Additionally, self-care does not only apply for individual care but in many contexts takes on forms of community-based and accompaniment models to care.
Self-care is about promoting individual and collective health and wellbeing. It includes self-awareness, self-testing and self-management of healthcare needs. (WHO, 2024).
Self-care Builds on Indigenous and Radical Resistance Traditions
In addition, we need to recognise that self-care isn’t a new method and that it builds on many indigenous and radical resistance traditions. Within indigenous health literature, self-care is approached as a continuum of healing inclusive of the wellbeing of people, communities and the planet and not as an individual act or a method. This relational practice of self-care aligns with the Indigenous ethical principle of collective flourishing or “living well.” (Dudgeon, Pat et al., 2023). In terms of self-care as an act of resistance, we need to acknowledge Audre Lorde when she famously said, “Caring for myself is not self-indulgence, it is self-preservation, and that is an act of political warfare.” (Audre Lorde, 1988). Understanding the traditions and history of self-care is important as we advance calls to accelerate the uptake of this rights-based and indigenous practice as a way for people to reclaim their rights, manage their health and wellbeing.
Caring for myself is not self-indulgence, it is self-preservation, and that is an act of political warfare.
The COVID Pandemic Accelerated Access to Self-care
For IPPF, self-care has been accelerated like many providers globally with the COVID pandemic where self-care was for some communities, marginalised groups and for specific health needs especially SRH needs was the only pathway to care. Self-managed abortion through medicine became the only way to access this lifesaving services. Based on IPPF 2024 annual performance review data, in all, 18 MAs reported data under this approach, with a total of 87,000 abortion self-care services - a substantial increase compared to the 21,000 abortion self-care services provided in 2023. Accelerated uptake of STI including HIV self-testing kits and HPV self-testing were sought and achieved during COVID-19 across different contexts, availing access to a service that is much needed and in a dignified and preferred way to the communities. The pandemic also cemented what we already knew is that when communities are empowered with the evidence-informed and accessible information about their health needs they have higher levels of adherence and can manage their conditions effectively and in some instances help prevent the spread of disease. We can't attribute all of this change to self-care but acknowledge that self-care is usually the preferred method for clients, its rights-based and for many sexual and reproductive health conditions including self-managed medical abortion is effective (IMAP statement, 2021).
Contraceptive self-care was there before the pandemic with self-injectables (DMPA- SC), oral contraceptive pills, and condoms but accelerated after the pandemic with more self-care options that are reliable and preferred by clients. As per IPPF service statistics, in 2024 member associations have distributed more than 1.4 million self-injectable service to clients globally which is a 28% increase from 2023. This data demonstrates that providers and clients see the value in investing and delivering self-care services as among the integrated package of essential services that IPPF Member Associations are delivering and widening access by ensuring they deliver services in-facility, digitally and with self-care options.

Let's acknowledge that self-care is usually the preferred method for clients
IPPF/Leki Lao/TongaCultivating the power of self-care for collective resistance within the sexual and reproductive health, rights and justice movement
At IPPF we believe that expanding access to self-care especially among young people in all their diversity is crucial and empowers them to take control of their health, make informed choices, and as a form of resistance. We support young people to access care including through self-care and digital health methods in a rights-based, stigma-free and pleasure positive approach that moves from the patriarchal, highly medicalised and stigmatising models care. This includes preventative measures, accessing healthcare, and managing potential issues like unwanted pregnancy or STIs.
As young people are three times more likely than older people to be unemployed (ILO, 2024), they are less likely to have resources to access the health services they need even in the event of an illness. Self-care would then be the only way to access the sexual and reproductive health services they need. However, with the rise of mis-information campaigns on sexual and reproductive health especially on the effectiveness and safety of medical abortion, vaccines among other services that are needed by young people, self-care without information and education campaigns are needed. Campaigns that promote positive narratives on medical abortion, effectiveness of vaccines, raising awareness of quality assured commodities and how to guides on self-care for SRH that are pleasure-positive, inclusive and using accessible language are important.
Self-care increases the community engagement with autonomy over their health and provides an opportunity for health systems to improve equitable access to healthcare, quality of care, and reduce out-of-pocket expenditure for communities.

We support young people to access care including through self-care and digital health methods
IPPF/Mercy Juma/KenyaAt times of financial constraints, Self-care is an opportunity and a cost-effective strategy
Self-care interventions, such as self-administered contraceptives and at-home diagnostic tests, can significantly lower healthcare costs and improve financial protection. By minimizing the need for facility-based services, these interventions reduce out-of-pocket expenses for users and alleviate the financial burden on healthcare systems. For instance, the use of over-the-counter emergency contraceptive pills without a prescription has been recommended to improve access and reduce costs.
Challenges such as limited awareness, cultural stigma, and inadequate access to resources can hinder the effectiveness of self-care interventions. Strategies to overcome these barriers include community education, policy reforms, and the integration of digital health tools to disseminate information and services.
Prioritizing SRHRJ within the UHC framework and enhancing it with self-care intervention creates a more inclusive, sustainable, and rights-based health system. SRHRJ must go beyond checkboxes; quality, equity, rights, and full spectrum inclusion (e.g., contraception, safe abortion, cancer screenings, STI treatment, gender-violence services) need systematic integration. Legislative, governance, and financial frameworks are required to allocate and sustain resources while promoting accountability for SRHR to achieve the UHC 2030 agenda.

"Being able to monitor my own blood pressure during pregnancy made me feel in control of my health."
AFGA / IPPFIn Afghanistan, one client told us “Being able to monitor my own blood pressure during pregnancy made me feel in control of my health. I could act quickly if something didn’t seem right". "With pregnancy self-testing, I could confirm my pregnancy early and seek the care I needed without waiting for an appointment”
These stories and many more call for moving away from medicalized and provider-led approaches to care to more people-centred and quality assured model of care that empowers individuals when supported by the community and providers when needed or required.